What Is The Difference Diabetes Type 1 And 2, Symptoms ⏬👇
What Is The Difference Diabetes Type 1 And 2
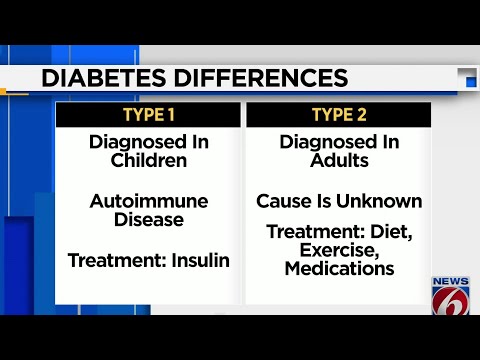
Diabetes, a chronic metabolic disorder, manifests in two primary forms: Type 1 and Type 2. These conditions differ fundamentally in their underlying causes and management. Type 1 diabetes results from an autoimmune response, where the body’s immune system attacks and destroys insulin-producing cells in the pancreas. In contrast, Type 2 diabetes typically develops due to insulin resistance and lifestyle factors. Understanding the distinctions between these two forms of diabetes is crucial for effective management and treatment.
Diabetes Type 1 And 2 Symptoms
Here are the common symptoms of Diabetes Type 1 and Type 2:
Type 1 Diabetes Symptoms:
- Excessive thirst and hunger
- Frequent urination
- Unexplained weight loss
- Fatigue
- Blurry vision
- Irritability
- Increased susceptibility to infections
Type 2 Diabetes Symptoms:
- Increased thirst and hunger
- Frequent urination
- Fatigue
- Blurry vision
- Slow-healing wounds or sores
- Recurring infections
- Tingling or numbness in hands or feet
- Dark patches on the skin
It’s important to note that some individuals with Type 2 diabetes may not exhibit any noticeable symptoms, making regular screenings and check-ups important, especially if there is a family history or other risk factors. If you or someone you know is experiencing these symptoms, it’s crucial to consult a healthcare professional for proper diagnosis and management.
Diabetes Type 1 And 2 Treatment
The treatment for Diabetes Type 1 and Type 2 differs due to the distinct underlying causes of these conditions. Here’s an overview of the treatment approaches for each:
Type 1 Diabetes Treatment:
- Insulin Therapy: Since Type 1 diabetes results from a lack of insulin production, individuals with this condition need insulin therapy. This typically involves multiple daily injections or the use of an insulin pump.
Type 2 Diabetes Treatment:
- Lifestyle Changes: For many people with Type 2 diabetes, managing the condition begins with lifestyle modifications. This includes adopting a balanced diet, increasing physical activity, and achieving and maintaining a healthy weight.
- Oral Medications: In some cases, oral medications may be prescribed to help the body use insulin more effectively or stimulate the pancreas to produce more insulin.
- Injectable Medications: For individuals who do not achieve glycemic control with oral medications, injectable medications like GLP-1 receptor agonists or insulin may be used.
- Regular Monitoring: Monitoring blood glucose levels is crucial for both Type 1 and Type 2 diabetes. It helps individuals and healthcare providers make necessary adjustments to treatment plans.
- Possible Insulin Therapy: In advanced cases of Type 2 diabetes, individuals may eventually require insulin therapy.
The treatment plan for each person with diabetes should be individualized, taking into account their specific medical history and needs. Consultation with a healthcare provider is essential to determine the most appropriate treatment approach and to effectively manage diabetes.
Diabetes Type 2 Diets
A healthy diet is a fundamental part of managing and controlling Type 2 diabetes. Here are some dietary guidelines and tips for individuals with Type 2 diabetes:
- Carbohydrate Control: Monitor your carbohydrate intake and choose complex carbohydrates with a low glycemic index, such as whole grains, legumes, and vegetables. Avoid or limit simple carbohydrates, including sugary snacks and beverages.
- Fiber-Rich Foods: Incorporate high-fiber foods like fruits, vegetables, and whole grains into your diet. Fiber helps stabilize blood sugar levels and promotes overall health.
- Lean Proteins: Include lean sources of protein, such as skinless poultry, fish, tofu, and legumes. Protein can help control hunger and maintain muscle mass.
- Healthy Fats: Opt for healthy fats like those found in avocados, nuts, seeds, and olive oil. Limit saturated and trans fats found in processed and fried foods.
- Portion Control: Be mindful of portion sizes to manage calorie intake and blood sugar levels.
- Regular Meal Schedule: Stick to a consistent meal schedule, and avoid skipping meals. This can help regulate blood sugar levels.
- Balanced Meals: Aim for balanced meals that include a variety of food groups, including carbohydrates, protein, and healthy fats.
- Limit Added Sugars: Minimize or eliminate sugary foods and drinks from your diet. Pay attention to food labels for hidden sources of added sugars.
- Stay Hydrated: Drink plenty of water to help maintain good overall health.
- Consult a Dietitian: Consider working with a registered dietitian who specializes in diabetes management to create a personalized meal plan.
Remember that there is no one-size-fits-all diet for individuals with Type 2 diabetes, and it’s crucial to work with a healthcare provider or a dietitian to develop a plan tailored to your specific needs and preferences. Monitoring your blood sugar levels and making adjustments to your diet based on your body’s response is also essential for effective management.
Glucose Levels For Type 2 Diabetes
Glucose level targets for individuals with Type 2 diabetes can vary depending on factors such as age, overall health, and individual circumstances. However, here are general guidelines for target glucose levels:
Fasting Blood Glucose (measured in the morning before eating):
- Target range: 80-130 mg/dL (4.4-7.2 mmol/L)
Postprandial Blood Glucose (measured 1-2 hours after a meal):
- Target range: Less than 180 mg/dL (10 mmol/L)
It’s important to note that these are typical target ranges, and individualized goals may be set by a healthcare provider. Some individuals may have stricter or more relaxed targets based on their specific health conditions and needs.
Regular monitoring of blood glucose levels is crucial to assess how well you are managing your diabetes and to make necessary adjustments to your treatment plan, including medications and dietary choices. Always consult with a healthcare provider or a diabetes educator to establish personalized glucose level goals and treatment plans that are appropriate for your situation.
Insulin Dependent Diabetes
Insulin-dependent diabetes, also known as Type 1 diabetes, is a chronic autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, individuals with Type 1 diabetes produce little to no insulin, a hormone essential for regulating blood sugar (glucose) levels.
Key characteristics of insulin-dependent diabetes (Type 1 diabetes) include:
- Insulin Dependency: Individuals with Type 1 diabetes must rely on insulin therapy to survive. This typically involves multiple daily injections of insulin or the use of an insulin pump.
- Onset: Type 1 diabetes often begins in childhood or adolescence, although it can develop at any age.
- Autoimmune Condition: It is an autoimmune disease, meaning the immune system mistakenly targets and damages the body’s own cells.
- Blood Sugar Management: Managing blood sugar levels is crucial for individuals with Type 1 diabetes. They need to monitor their blood glucose regularly and adjust insulin doses to maintain optimal levels.
- Diet and Lifestyle: A healthy diet and regular physical activity are important for managing blood sugar levels. Carbohydrate counting and meal planning are common practices.
- Complications: If not well-managed, Type 1 diabetes can lead to various complications, including heart disease, kidney problems, neuropathy, and eye issues.
- Continuous Monitoring: Some individuals may use continuous glucose monitors (CGMs) to track their blood sugar levels in real time.
Treatment and management of insulin-dependent diabetes require close collaboration with healthcare providers, including endocrinologists, diabetes educators, and dietitians. Type 1 diabetes management aims to maintain blood sugar levels within a target range to reduce the risk of complications and improve overall quality of life for those living with the condition.
Managing Type 2 Diabetes
Managing Type 2 diabetes involves a combination of lifestyle changes, medication when necessary, and regular monitoring. Here are some key strategies for effectively managing Type 2 diabetes:
- Healthy Eating:
- Follow a balanced and nutritious diet.
- Control portion sizes.
- Choose foods with a low glycemic index, such as whole grains, fruits, and vegetables.
- Limit sugar and refined carbohydrates.
- Regular Physical Activity:
- Engage in regular exercise, such as brisk walking, swimming, or cycling.
- Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
- Weight Management:
- Achieve and maintain a healthy weight.
- Weight loss can improve insulin sensitivity and blood sugar control.
- Medication, if Prescribed:
- Some individuals with Type 2 diabetes may require oral medications or insulin to help control blood sugar levels.
- Take medications as prescribed and follow your healthcare provider’s recommendations.
- Blood Sugar Monitoring:
- Check your blood sugar levels regularly, as advised by your healthcare provider.
- Keep a record of your readings to identify patterns and trends.
- Regular Medical Checkups:
- Visit your healthcare provider for regular checkups and diabetes management reviews.
- Stress Management:
- Practice stress-reduction techniques, as stress can affect blood sugar levels.
- Quit Smoking:
- If you smoke, quitting can improve your overall health and reduce the risk of complications.
- Education and Support:
- Learn about diabetes management through educational programs or classes.
- Seek support from healthcare professionals, diabetes educators, and support groups.
- Foot Care:
- Inspect your feet daily for any cuts, sores, or other issues.
- Wear comfortable, well-fitting shoes.
- Eye and Dental Care:
- Regularly see an eye specialist and a dentist to monitor and address potential diabetes-related complications.
Managing Type 2 diabetes is a lifelong commitment, and it’s essential to work closely with your healthcare team to create a personalized management plan. This plan should be regularly reviewed and adjusted as needed to achieve and maintain target blood sugar levels and reduce the risk of complications.
Type 1 Diabetes Symptoms
The symptoms of Type 1 diabetes can develop relatively quickly and are often more pronounced than those of Type 2 diabetes. Common symptoms of Type 1 diabetes include:
- Excessive Thirst (Polydipsia): Individuals may experience intense thirst and an increased need to drink fluids.
- Frequent Urination (Polyuria): An increased need to urinate, even during the night, is a common symptom.
- Unexplained Weight Loss: Despite eating more, unexplained weight loss can occur. This is due to the body breaking down fat and muscle for energy when it can’t use glucose effectively.
- Extreme Hunger (Polyphagia): A significant increase in appetite can be a sign of Type 1 diabetes.
- Fatigue: Individuals may feel unusually tired or weak.
- Blurry Vision: Blurred vision can result from high blood sugar levels.
- Irritability: Mood changes, such as irritability and mood swings, can occur.
- Yeast Infections: An increased susceptibility to yeast infections, especially in women, can be a symptom.
- Ketoacidosis: In severe cases, diabetic ketoacidosis (DKA) can develop, leading to symptoms such as deep and labored breathing, a fruity odor on the breath, and confusion. DKA is a medical emergency.
If you or someone you know is experiencing these symptoms, especially if they are severe or rapidly worsening, it’s essential to seek immediate medical attention. Type 1 diabetes is typically diagnosed through blood tests to measure glucose and ketone levels. Early diagnosis and treatment are crucial for managing the condition and preventing complications.
Type 1 Diabetes Treatment
The primary treatment for Type 1 diabetes involves the replacement of insulin, as the body is unable to produce this hormone naturally. Proper management of Type 1 diabetes is essential for maintaining blood sugar levels within a target range and preventing complications. Here are key aspects of treatment for Type 1 diabetes:
- Insulin Therapy: Individuals with Type 1 diabetes require lifelong insulin therapy. This therapy can be administered in several ways:
- Multiple Daily Injections: Insulin is injected multiple times a day using syringes, insulin pens, or insulin pumps.
- Insulin Pump: An insulin pump delivers a continuous supply of insulin throughout the day, with the option to adjust doses as needed.
- Continuous Glucose Monitor (CGM): CGMs provide real-time information about blood sugar levels, helping individuals adjust insulin doses and make more informed decisions.
- Blood Sugar Monitoring: Regular monitoring of blood glucose levels is essential. This involves checking blood sugar levels multiple times a day, especially before meals and at bedtime. Monitoring helps determine the appropriate insulin doses.
- Carbohydrate Counting: Learning to count carbohydrates and understanding how they affect blood sugar levels is crucial. This enables individuals to adjust insulin doses based on their food intake.
- Healthy Eating: Following a balanced diet is vital. A registered dietitian can help create a meal plan that aligns with blood sugar goals. Focus on complex carbohydrates, fiber-rich foods, and portion control.
- Regular Physical Activity: Regular exercise is important for blood sugar control and overall health. Consult with a healthcare provider to create an exercise plan.
- Insulin Adjustment: Insulin doses need to be adjusted based on factors such as food intake, physical activity, illness, and stress. This should be done in consultation with a healthcare provider.
- Regular Medical Checkups: Regular visits to healthcare providers are crucial for diabetes management. These checkups can help assess overall health, monitor for complications, and make necessary treatment adjustments.
- Education and Support: Diabetes self-management education and support programs can provide valuable information and resources for individuals and their families.
- Continuous Monitoring: Continuous glucose monitoring (CGM) and/or flash glucose monitoring systems can provide real-time information about blood sugar levels, helping with proactive management.
It’s important to work closely with healthcare providers, diabetes educators, and registered dietitians to create a personalized treatment plan. This plan should be regularly reviewed and adjusted to maintain target blood sugar levels, prevent complications, and improve overall quality of life for individuals with Type 1 diabetes.
Type 1 Diabetes Versus 2
Type 1 diabetes and Type 2 diabetes are two distinct forms of diabetes with different causes, characteristics, and treatment approaches. Here are the key differences between Type 1 and Type 2 diabetes:
Type 1 Diabetes:
- Cause: Type 1 diabetes is an autoimmune condition where the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This leads to a complete lack of insulin production.
- Age of Onset: It often develops in childhood or adolescence, but it can occur at any age.
- Insulin Dependency: Individuals with Type 1 diabetes are entirely dependent on insulin therapy to survive. They need multiple daily injections or an insulin pump.
- Risk Factors: There are genetic and environmental factors that contribute to the risk of developing Type 1 diabetes, but the exact cause is not fully understood.
- Body Weight: People with Type 1 diabetes can have a healthy weight or be underweight.
- Lifestyle Role: Lifestyle factors have a minimal impact on the development of Type 1 diabetes.
Type 2 Diabetes:
- Cause: Type 2 diabetes is primarily associated with insulin resistance, where the body’s cells do not respond effectively to insulin, and a relative insulin deficiency over time. Genetic and lifestyle factors play a significant role.
- Age of Onset: It typically develops in adulthood, although it is becoming more common in children and adolescents.
- Insulin Dependency: Initially, people with Type 2 diabetes may not need insulin therapy, but it can become necessary as the condition progresses.
- Risk Factors: Risk factors for Type 2 diabetes include genetics, obesity, physical inactivity, poor diet, and other lifestyle choices.
- Vücut Ağırlığı: Tip 2 diyabetli kişilerin çoğu aşırı kilolu veya obezdir, ancak sağlıklı kiloya sahip kişilerde de ortaya çıkabilir.
- Yaşam Tarzı Rolü: Diyet ve egzersizi de içeren yaşam tarzı değişikliklerinin Tip 2 diyabetin gelişimi ve yönetimi üzerinde önemli bir etkisi olabilir.
Özetle Tip 1 diyabet, genellikle çocukluk çağında başlayan, tanıdan itibaren insülin tedavisi gerektiren ve bilinen bir önleme yöntemi olmayan bir otoimmün hastalıktır. Tip 2 diyabet sıklıkla insülin direnciyle ilişkilidir ve yetişkinlikte gelişebilir. Diyet ve egzersizi de içeren yaşam tarzı değişiklikleri, Tip 2 diyabetin tedavisinde ve önlenmesinde önemli bir rol oynamaktadır. Her iki diyabet türü de sağlıklı kan şekeri seviyelerini korumak ve komplikasyonları önlemek için düzenli izleme ve yönetim gerektirir.
Diyabet Tablosu İçin Kan Şekeri Seviyeleri
Diyabet için kan şekeri seviyeleri tipik olarak dekilitre başına miligram (mg/dL) veya litre başına milimol (mmol/L) cinsinden ölçülür. Aşağıdakiler diyabetli kişiler için genel kan şekeri düzeyi kurallarıdır:
Açlık kan şekeri için (en az 8 saat hiçbir şey yemeden veya içmeden sonra ölçülür):
- Normal: 100 mg/dL’den (5,6 mmol/L) az
- Prediyabet (bozulmuş açlık glikozu): 100-125 mg/dL (5,6-6,9 mmol/L)
- Diyabet: 126 mg/dL (7,0 mmol/L) veya daha yüksek
Yemekten 1-2 saat sonra (yemek sonrası) ölçülen kan şekeri düzeyleri için:
- Normal: 140 mg/dL’den (7,8 mmol/L) az
- Prediyabet: 140-199 mg/dL (7,8-11,0 mmol/L)
- Diyabet: 200 mg/dL (11,1 mmol/L) veya daha yüksek
Bunların genel kurallar olduğunu ve bireysel kan şekeri hedeflerinin yaş, genel sağlık durumu ve kişiselleştirilmiş tedavi planları gibi faktörlere göre değişebileceğini lütfen unutmayın. Diyabetli kişilerin, durumu etkili bir şekilde yönetmek ve komplikasyonları önlemek amacıyla kişiselleştirilmiş kan şekeri düzeyi hedefleri ve tedavi hedefleri belirlemek için sağlık uzmanlarıyla birlikte çalışmaları çok önemlidir. Ayrıca kan şekeri seviyeleri dalgalanabilir, bu nedenle sağlıklı seviyeleri korumak için düzenli izleme kritik öneme sahiptir.



